
PQRS is one step in the newly consolidating reporting requirements that significantly impact Physician Medicare revenue.
Did you know that how you follow the Physician’s Quality Reporting System (PQRS) in 2016 will have a significant impact on your practice revenue in coming years? CMS has stated that failure to comply will cut your Medicare reimbursement by 2% starting in 2018. Further, tomorrow, March 22, is a deadline that if missed can carry a 6% penalty.
Eagle advises that, 2016 is the last reporting year for these three separate programs. During 2016, CMS will release rules to implement the MACRA legislation, which will consolidate all three of these programs into a new program called the Merit-Based Incentive Payment System (MIPS). And, under the consolidation, the penalties are designed to increase, year over year. The Hospitalist makes this clear in a recent article:
“As the Medicare physician payment system moves toward value-based payment, hospitalists must report quality measures in the Physician Quality Reporting System (PQRS) or face ever-increasing penalties.”
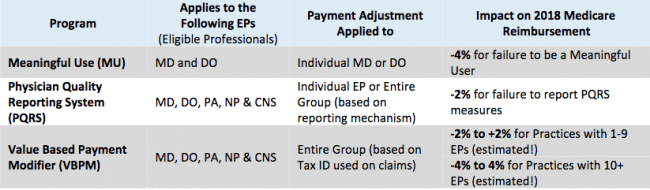
Negative impacts on practices from Eagle’s report on Medicare Incentive Programs: 2016 & Beyond. Write to us for details.
As you can see from the table above (contact us for more information), PQRS is part of a systematic reporting system being consolidated under new and evolving government policies. These policies are designed to inspire both cost cuts, and also increase the value of patient care.
During 2016 for PQRS, CMS explains, “In order for EPs to satisfactorily report PQRS measures, EPs or group practices are required to report one cross-cutting measure if they have at least one Medicare patient with a face-to-face encounter. A cross-cutting measure is defined as a measure that is broadly applicable across multiple providers and specialties. The Centers for Medicare & Medicaid Services (CMS) defines a face-to-face encounter as an instance in which the EP billed for services such as general office visits, outpatient visits, and surgical procedure codes under the Medicare Physician Fee Schedule (MPFS). CMS does not consider telehealth visits as a face-to-face encounter.”
The 2016 PQRS program specifies 280 quality measures. Providers select 9 measures across 3 domains that are applicable to their practice to report. CMS has released a new tool to assist providers in finding appropriate PQRS measures. You may also find the guide CMS Guide (PDF) on reporting helpful.
Eagle consultants will be pleased to review your practice needs for PQRS and provide a quote on experienced guidance and solutions.

