Quality Payment Programs, the final rule
The Quality Payment Program final rule has been released. What payment adjustments will physicians see in the upcoming years? How quickly will the new payment methodologies be implemented?
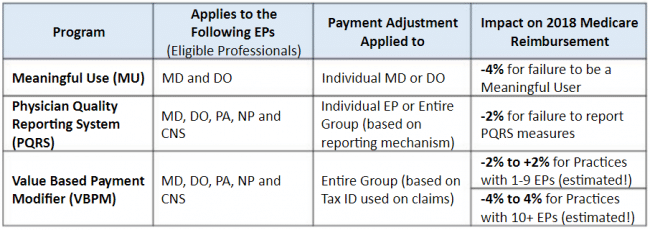
Read MoreCMS Quality Payment Programs are a key element of CMS’ effort to transform the Medicare system from a “Pay for Volume” model to “Pay for Value”. The Quality Payment Programs include Alternative Payment Models (APMs) such as ACOs and Patient Centered Medical Homes (PCMH). For physician practices not participating in an APM, the Merit-Based Incentive Payment System (MIPS) will apply. MIPS, which will be effective 1/1/2017, incorporates the legacy Meaningful Use, PQRS and Value Modifier programs.
The Quality Payment Program final rule has been released. What payment adjustments will physicians see in the upcoming years? How quickly will the new payment methodologies be implemented?
Read More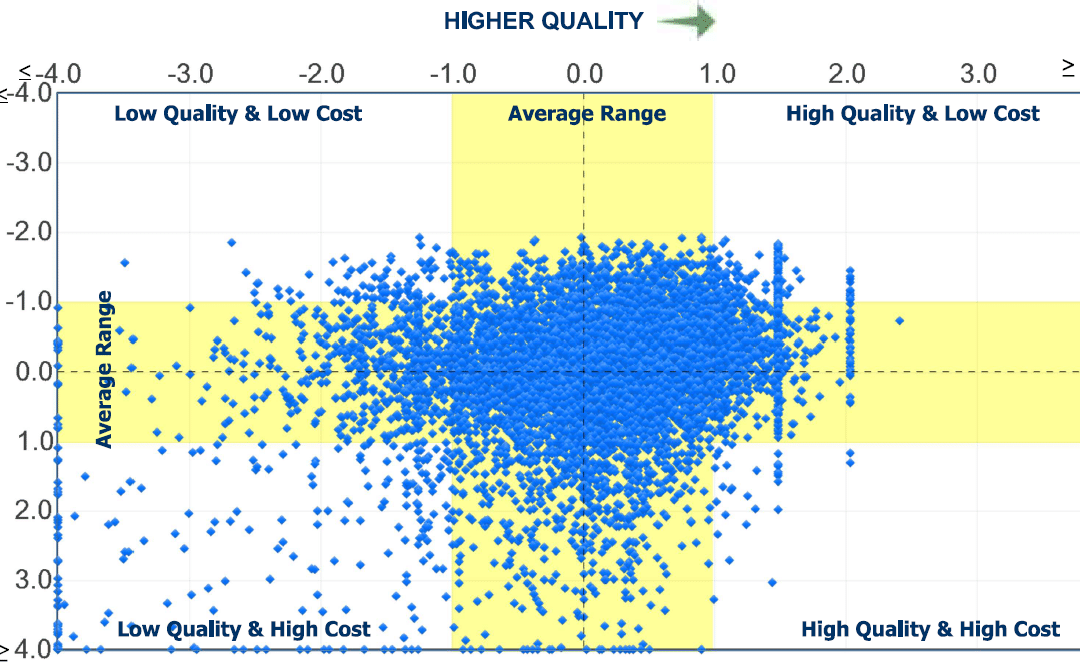
The 2015 QRUR have been released. Practices can download them and learn about their potential payment adjustments in 2017. They can also begin to understand how to perform well in MIPS.
Read More
Meaningful Use is still on for 2016 and 2017. Learn what Acting Administrator has said about Meaningful Use and the MACRA implementation.
Read More