On October 14, the Centers for Medicare and Medicaid services (CMS) released the 2,400 page final rule for the Quality Payment Program (QPP). This rule defines the programs outlined in the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA). The QPP was created by congress to replace the Sustainable Growth Rate (SGR). The two tracks are the Merit-based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (Advanced APMs). The MIPS will apply to most physicians, but the ultimate goal of the program is to have most providers participate in Advanced APMs.
Incentives / Penalties for QPP
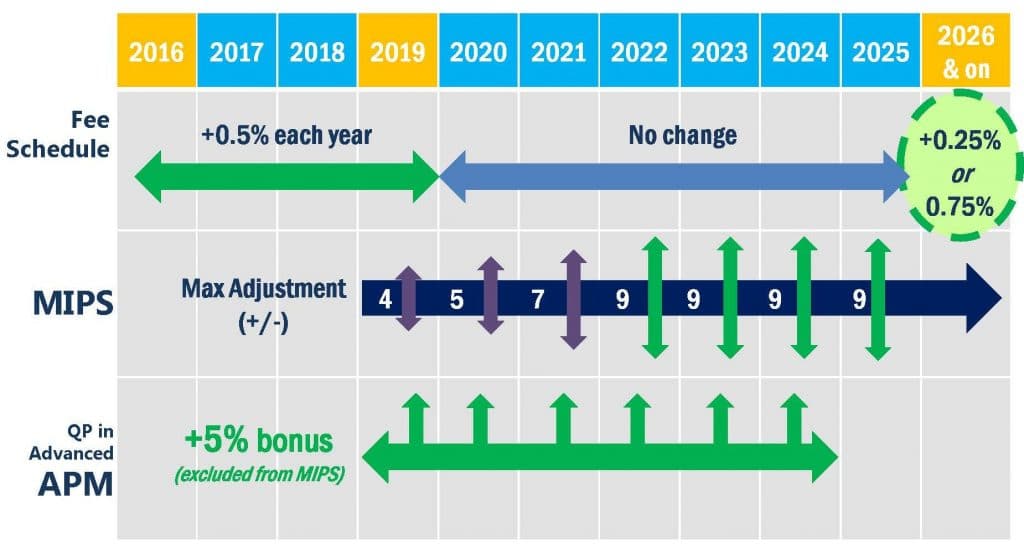
For the MIPS, providers will be subject to a graduated incentive/penalty system that will mean providers may see penalties from -9% of Medicare reimbursements to incentives of up to +37% of Medicare reimbursements. MIPS replaces the Meaningful Use program, Physician Quality Reporting System (PQRS), and Value Modifier programs. The other QPP, Advanced APMs, means a 5% incentive payment for Medicare reimbursements for those providers who participate and are considered a Qualifying APM Participant (QP). Those who are currently participating in an APM are not necessarily guaranteed to be a QP for 2017.
Merit-based Incentive Payment System in 2017
After a lot of push back on the proposed rule in May, CMS has made 2017 and 2018 measurement years transition years. In 2017, providers will only have to report minimal data to MIPS to avoid the penalty. However, for providers who have already implemented CEHRT and are comfortable reporting to PQRS, there is the real possibility of receiving an incentive bonus from MIPS. Clinicians who report data in all of the performance categories can achieve a higher performance score and possibly achieve over the 70 points exceptional performance threshold. The ONC has stated that practices that submit data for the full year will have the best chance at receiving a moderate bonus. It’s also important to note that although it will be easy to avoid a payment penalty this year, the standard will most likely not be as low this year. Learning how you will perform, by performing to the best of your ability will help you to know how you may size up against next year’s benchmarks.
Learn more about the Quality Payment Program:
CMS Quality Payment Program website
Eagle Quality Payment Program posts
Editor’s Note: Subsequent to the publication of this article, CMS has renamed the “Meaningful Use” programs and MIPS “Advancing Care Information” category to “Promoting Interoperability”.

