Editor’s Note: Subsequent to the publication of this article, CMS has renamed the “Meaningful Use” programs and MIPS “Advancing Care Information” category to “Promoting Interoperability”.
For 2016 the three Medicare Incentive programs — Meaningful Use, PQRS and the Value-Based Payment Modifier apply to physician practices. As is usually the case, the rules have been updated. In this post, we will discuss the first of these three programs, Meaningful Use.
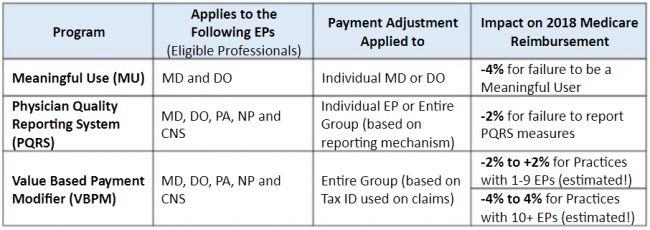
This chart shows the breakdown of Medicare Incentive Programs for 2016 and beyond.
Medicare Meaningful Use Incentives for 2016
During early 2016 CMS acting director Andy Slavitt set off a firestorm with his comments which suggested that the Meaningful Use program was over. It took only a few days for the backpedaling to begin with a series of clarifications. In short, Meaningful Use remains active for all of 2016:
- All physicians must utilize a set of Stage 2 measures which consist of a combination of the prior “Stage 1” and “Stage 2” measures. In October of 2015, CMS released a final rule that outlines the latest version of the new Stage 2 which includes 10 objectives.
- New Physicians may report for a 90-day period, but physicians not new to Meaningful Use must report for a full twelve months.
- Meaningful Use program will only have incentive payments for one more year, 2016. All physicians that started MU in 2012 or 2013, $2000 per physician is the 2016 incentive. Those who began in 2014 will receive $4000. If a physician began before 2011 or after 2014, they are no longer eligible for incentives under MU.
Noteworthy Stage Two Objectives
Objective #1: Privacy and Security Objective – this objective will be the most likely culprit that will cause physicians to fail audits. A requirement of this objective is a study known as the HIPAA Security Risk Analysis (SRA), which needs to be completed between the first day of 2016 and the attestation date early in 2017.
Objective #5: Health Information Exchange – this objective requires 10 percent of your outgoing referrals to include coordination with physicians that you refer patients to or transmit a summary of care record to. This measure does not include electronic faxes. This objective will be challenging for many physicians because it requires cooperation between practices. Don’t put this one off – best to get it done early in the year!
Objective #10: Public Health Reporting – this objective is not written clearly and will be a cause for confusion for many physicians. There are two registries physicians must submit to for this measure. Registry intent with a physician’s appropriate registry or registries had to be completed by the last day of February 2016. Physicians may report the MU Clinical Quality Measures (CQMs) and comply with PQRS program via their EHR system.
Need a little direction to ensure you are meeting all these new objectives for 2016? Reach out to us today and we would be happy to discuss how we can help you keep your practice in compliance. Next up: PQRS.

