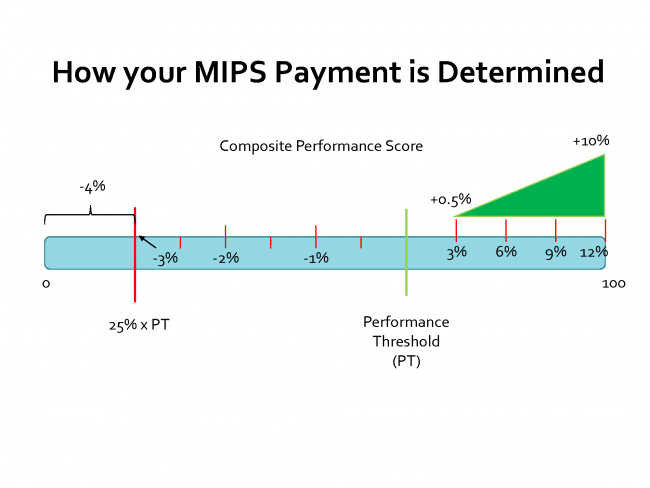
As we mentioned in our initial post (What the MIPS?), the payment modifier for MIPS will be determined by a performance threshold (PT) set by CMS and your individual or group Composite Performance Score (CPS). This CPS is a number between 0 and 100 is calculated by weighting the scores attained in 4 performance categories.
The PT for the first couple of years of MIPS will be determined by CMS from past incentive program data. They are going to make an educated guess as to where to place the PT such that half of clinician payments would be attributed to clinicians with scores higher than the PT and half with scores lower than the PT. MIPS is designed to be budget neutral. CMS will use the penalty money from the low-scoring clinicians and groups to pay the incentive payments for the high-scoring. After the first couple of years, CMS will use the mean or median CPS to determine this threshold.
How is the payment modifier determined?
This is where it gets complicated. Although CMS set out to make the payment adjustment predefined, the positive incentive can be challenging to understand. The negative payment adjustment is straightforward. If a group or individual clinician’s score falls is lower than the PT there will be a negative payment adjustment. If the score is very low, below 25% of the PT, the clinician or group will be automatically subject to the full penalty. In 2017 that penalty will be 4% of the Medicare fee. Those falling between 25% of the PT and the PT will be subject to negative payment adjustment between 3% and 0% on a linear scale. This means there is a sliding scale for the negative adjustment and not just discrete adjustments (such as categories for 3%, 2%, and 1%).
On the positive side, clinicians will receive positive payment adjustments between 0% and 4% on a linear scale in 2017. These payment adjustments have a multiplicative factor of X (up to 3) similar to the VM program. This factor means that clinicians could receive up to 12% positive adjustments of their Medicare claims. There is an additional positive adjustment for clinicians for scores above the 25th percentile of possible scores in the range above the PT of up to 10%. For example, if the PT=60, those clinicians with a CPS of 70 or greater would receive the additional positive adjustment. A clinician with a CPS of 100 could receive up to a 22% positive payment adjustment for MIPS in the first year!
 How are performance category scores weighted?
How are performance category scores weighted?
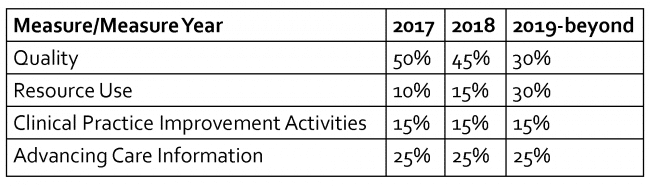
For 2017 performance category scores will be weighted with the emphasis on the Quality performance category. The Quality performance category will be worth half of the total CPS. The other categories will be weighted as seen below. Over the course of 3 years the weighting will shift the focus from Quality to Resource Use. The other two performance categories will remain the same. CMS has stipulated that if they deem that Meaningful Use of CEHRT has been achieved by at least 75% of clinicians, they may lower the Advancing Care Information performance category to a minimum of 15%.
Not all clinicians’ scores will be weighted the same way. CMS has reserved the right to re-weight performance categories for clinicians who don’t have sufficient data for a performance category, who are not subject to participating in a category or who are participants in a MIPS APM entity.
To learn more about how individual categories are scored and measured please look for our other blog posts on the subject.
Editor’s Note: Subsequent to the publication of this article, CMS has renamed the “Meaningful Use” programs and MIPS “Advancing Care Information” category to “Promoting Interoperability”.