
Are you prepared for the changes from CMS for your clinician Quality Performance Program and reviews?
Editor’s Note: Subsequent to the publication of this article, CMS has renamed the “Meaningful Use” programs and MIPS “Advancing Care Information” category to “Promoting Interoperability”.
Eagle has reviewed the proposed changes by CMS (Centers for Medicaid and Medicare Services) to the Quality Payment Program for 2018, called “ Medicare Program; CY 2018 Updates to the Quality Payment Program” and added the new sections into this document so you may proactively assess how the proposed changes might affect your practice.
According to CMS, “The Quality Payment Program makes Medicare better by helping you focus on care quality and the one thing that matters most – making patients healthier. The Quality Payment Program ends the Sustainable Growth Rate formula and gives you new tools, models, and resources to help you give your patients the best possible care. You can choose how you want to take part based on your practice size, specialty, location, or patient population.”
The Quality Payment Program combines the existing Medicare Meaningful Use (MU), Physician Quality Reporting System (PQRS), and Value-Based Modifier (VBM) programs into MIPS, starting with the 2017 performance year. MIPS payment adjustments are applied to Medicare Part B payments two years after the performance year. 2019 is the payment adjustment year for the 2017 performance year.
Eagle consultant Phil Williams advises, “now it’s easier to avoid penalties, but to earn incentives you will have to do more work.” You now have to choose the right measures to report to earn incentive.
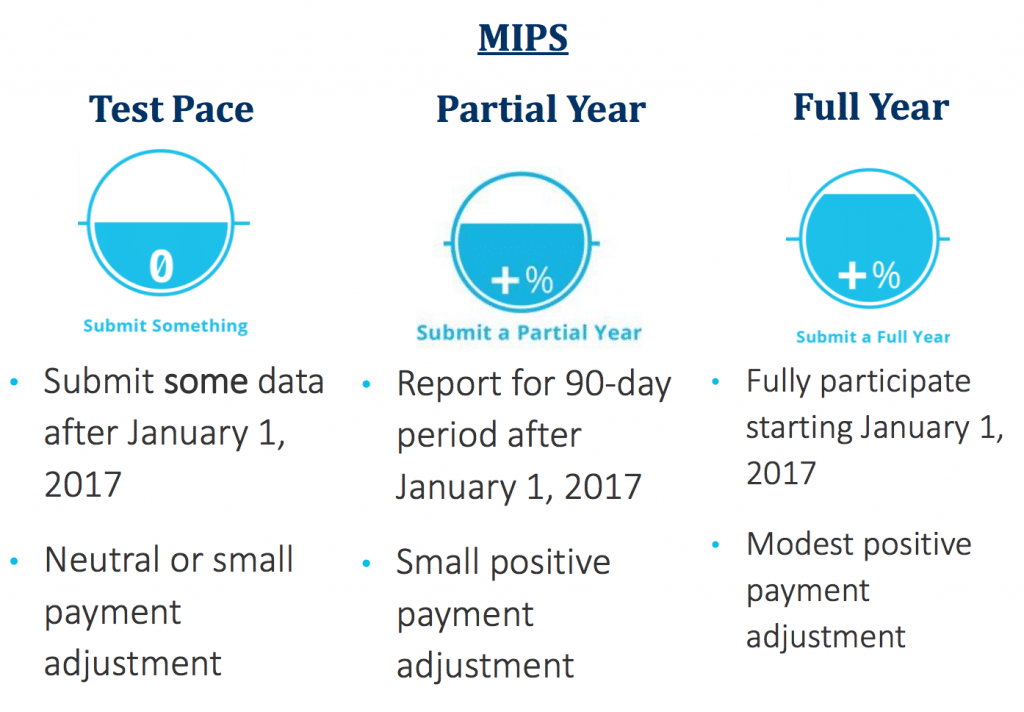
Time to get started on your clinician Quality Performance Program. Not participating in the Quality Payment Program for the transition year will result in a negative 4% payment adjustment.
The Quality Performance Category will continue to be weighted the highest in 2018. The quality measure scores are based on a combination of billable services and diagnoses, using HCPCS and ICD-10 codes. Clinicians can submit quality data to CMS in multiple methods.
Note that you have through October 2, 2017 to get ready and start the program. You can download the updated rule from Eagle with proposed changes right now and review.
Williams also notes that in Eagle’s experience, the practice and office manager usually “knows medical billing practices, and know how to submit information to the program, but they do not necessarily know how to efficiently maximize their score.”
Eagle specializes in maximizing incentive payments for physicians practices and hospitals with a focus on the MIPS program from CMS. Contact us today — (216) 503-0333.

