Editor’s Note: Subsequent to the publication of this article, on May 4, the House of Representatives passed an updated version of the American Health Care Act. The Senate has begun a review which is expected to result in significant revisions. CMS has also renamed the “Meaningful Use” programs and MIPS “Advancing Care Information” category to “Promoting Interoperability”.
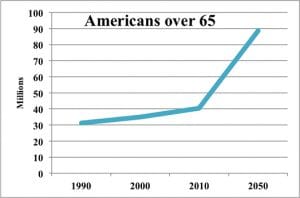 The first quarter of 2017 has brought us a lot of questions as to the future of healthcare and Medicare. But there are somethings that we know for sure. As Baby Boomers get older, approximately 10,000 become eligible for Medicare each day. As the number on Medicare increases the ratio of workers paying for those Medicare beneficiaries gets smaller, which increases the burden on those working. Health care expenditures accounted for 17.8% of GDP in 2015 which represents a 5.8% increase over the previous year. For the first time in over 2 decades, the US life expectancy has dropped, signs that Americans are sicker and more costly to care for. These non-partisan facts challenge any administration – Democratic or Republican. Medicare expenses will skyrocket, placing tremendous strains on the entire federal budget, unless program changes are made.
The first quarter of 2017 has brought us a lot of questions as to the future of healthcare and Medicare. But there are somethings that we know for sure. As Baby Boomers get older, approximately 10,000 become eligible for Medicare each day. As the number on Medicare increases the ratio of workers paying for those Medicare beneficiaries gets smaller, which increases the burden on those working. Health care expenditures accounted for 17.8% of GDP in 2015 which represents a 5.8% increase over the previous year. For the first time in over 2 decades, the US life expectancy has dropped, signs that Americans are sicker and more costly to care for. These non-partisan facts challenge any administration – Democratic or Republican. Medicare expenses will skyrocket, placing tremendous strains on the entire federal budget, unless program changes are made.
Future for the Affordable Care Act
The political focus during the beginning of the Trump administration has been on Obamacare, aka the Affordable Care Act (ACA). The future of the ACA is now uncertain. After campaigning for 7 years on repealing the ACA, winning the White House and majorities in both the House and Senate, and passing 50 repeal bills in the House during the Obama presidency, the GOP has failed to produce a bill to capture enough votes to pass even the House. The American Health Care Act (AHCA) attempted to roll back the taxes and penalties of the ACA and while also changing the ACA subsidies based on income to tax credits based on age. The AHCA also removed the provision for the “10 Essential Health Benefits,” while maintaining adult children’s access to parent’s plans until age 26. The bill was killed ostensibly by the House Freedom Caucus, a group of conservative law makers who felt that the AHCA did not go far enough or quick enough to roll back Medicaid expansion and other provisions they saw as government overreach.
Some house members, including Freedom Caucus member Jim Jordan of Ohio, believe that a clean repeal bill should be voted on. However, Speaker Ryan has indicated that the time for action health care has passed, declaring “Obamacare is the law of the land.” The White House has also sent signals that they are moving towards their next hurdle:Tax Reform. President Trump’s Chief of Staff, Reince Priebus, has even suggested working across the aisle because of their upset with the Freedom Caucus’s unwillingness to negotiate.
Medicare’s Quality Payment Program
The Trump administration and Congress have spent little or no time regarding any change of direction for the Medicare program. The Final Rule for the Quality Payment Program (QPP) was released in October 2016. The QPP Final Rule created the structure for the implementation of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA). The Final Rule, at over 2,400 pages long, didn’t cover all topics for the future years of the QPP, but attempted to lay the groundwork for 2017 and 2018. As eligible clinicians transition from PQRS, Meaningful Use, and the Value-based Payment Modifier programs, there are still plenty of unanswered questions about specifics for the program. The good news is, for the initial years under MIPS, most clinicians will be able to avoid penalties, by just reporting minimal information to CMS.
On its face, the QPP is designed to promote “quality” over “quantity.” The reality is, however, that the MACRA was passed with overwhelming bipartisan support to slow the growth of Medicare spending. Total Medicare spending is expected to almost double by 2025. Although the intention behind passing MACRA was to slow the rate of growth in Medicare spending, the CBO estimated that MACRA would only save $900 million over the course of 2015-2025 as compared to a plan to keep reimbursements flat. It remains to be seen how costs will shake out. The MIPS program will implement the Resource Use performance category in 2018.
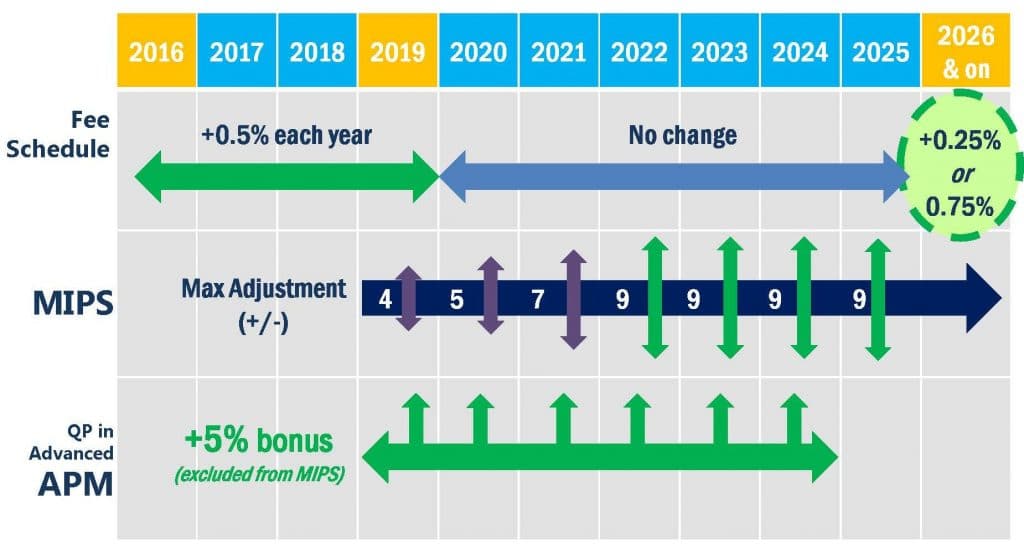
There is real opportunity for practices that get on board early with MIPS and Advanced Alternative Payment Models (Advanced APMs). Clinicians participating in Advanced APMs will see bonus lump sum payments of 5% of their Medicare reimbursements, combined with additional payments based on the details of the specific innovation model. Clinicians participating in MIPS could see a theoretical maximum 37% in increased Medicare reimbursements. It is important to note that practices who excelled in the early years of the Medicare Value-based Payment Modifier program earned, in one year, a massive 30%+ Medicare incentive bonus. There is a similar possibility for a big payday under the MIPS program, which would favor those who invest early in learning how to maximize their performance under this new program.
Eagle Consulting Partners offers its MIPS / MACRA Services to providers who desire assistance with eliminating penalties and maximizing incentive payments.

