The MIPS rules are complex and this complexity creates many opportunities to make mistakes. Here are 5 mistakes we have seen and our advice for avoiding them:
1. Filing the Promoting Interoperability (PI) hardship exception without evaluating the impact
In 2018, CMS introduced a flexibility for small practices (defined as 15 or fewer clinicians): the promoting interoperability hardship exception. This was a welcome change for many practices. By filing the exception, you free yourself from the PI category entirely. This includes an exemption from the MIPS-required security risk assessment. When you file for the hardship exception, the 25 percent of your final score for PI will be reallocated to the quality category, which will increase from 50% of the final score to 75% of the final score. 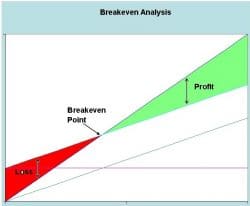
If you are earning a great Quality score, filing the hardship exception is a good idea. But if your quality score is low, your overall MIPS score (and bonus) may be lower as a result.
Avoid this MIPS mistake by performing a break-even analysis using our MIPS Promoting Interoperability Calculator. This calculator will show your expected MIPS bonus with or without filing for the Promoting Interoperability exception. After running the calculator you will need to compare the differences in any difference to the costs of complying with the Promoting Interoperability category, and then choose whichever option maximizes your practice return on investment.
2. Blindly trusting your vendor or the internet
Be cautious when relying on your vendors, registries or even government websites to provide you with MIPS updates. The only constant in the program is change. Some vendors have not updated their MIPS dashboards to reflect 2019 quality benchmarks. When vendors are late with updates to their systems, the scores presented to you are false representations of where you currently stand. This is just one example of out of date information that could easily fool you.
Avoid this top MIPS mistake by always verifying your sources and double-checking the date on which it was posted.
Government websites are not always up to date, either! Verify all your sources, even if they are .gov! When necessary, consult the actual text of the latest MIPS rule as published in the Federal Register. For an easy-to-read copy of the MIPS rules effective in 2019, click here.
3. Overlooking topped out measures
 Each year, CMS will deem certain quality measures “topped out”. When CMS determines that measures are too easy to achieve, they typically award only 7 points (instead of 10) for the highest performers. This becomes an issue when it is not properly planned for. as your final score could be disappointing. Consequently, topped out measures will eventually be removed from the program completely, so they must be replaced!
Each year, CMS will deem certain quality measures “topped out”. When CMS determines that measures are too easy to achieve, they typically award only 7 points (instead of 10) for the highest performers. This becomes an issue when it is not properly planned for. as your final score could be disappointing. Consequently, topped out measures will eventually be removed from the program completely, so they must be replaced!
Avoid this MIPS mistake by reading CMS regulatory updates as they are released and plan accordingly.
4. Ignoring your multiple practice settings
You must collect and submit data on at least 60 percent of your eligible cases (patients that meet the denominator criteria) to earn credit in the quality category. This includes all patients seen under your tax ID number—across all practice locations. If you see patients at 2 clinics that bill under the same TIN, you must collect and submit data on at least 60 percent of all the total denominator-eligible cases. If you fail to meet the 60 percent threshold, you will earn only 3 out of 10 points for that measure.
Example: You practice both in your office and at a hospital rehab department. You see 50% of total patients in your office, and the other 50% of patient visits at the hospital rehab department. You use your electronic record system in your office submitted a perfect score for quality measure 226. However, since you used the hospital’s EHR for those at their rehab department, you only submitted data for 50% of your eligible patients. You thus failed to meet the 60% case minimum, and receive 3 points for this quality measure instead of the perfect 10 points you were expecting.
Avoid this top MIPS mistake by integrating your data collection systems. Sometimes, there may be the option to adjust CPT coding to avoid triggering the quality measure criteria.
5. Hastily deciding on group/individual submission
Making a hasty decision regarding group vs individual reporting can prove detrimental to your final score; it is important to first do a thorough analysis to determine the most beneficial form of submission.
Example: Practice ABC has 2 clinicians: 1 physician and 5 nurse practitioners. The physician’s Medicare billing is over $1M while while each of the nurse practitioners bill $80,000 in Medicare. Since the nurse practitioners are all below the $90,000 MIPS threshold, they are exempt from MIPS. The seemingly easy decision is to submit MIPS data only for the doctor. In this scenario, suppose the doctor achieves a score of 74 out of 100 possible points. She will have avoided the penalty, but her Medicare bonus amounts will be negligible. However, suppose that all nurse practitioners had collected quality data perfectly and had achieved the maximum MIPS scores. MIPS permits exempt clinicians to participate if they choose. So If the practice submitted as a group, the MIPS score would be calculated on the combined total. In this hypothetical example, the overall practice MIPS score was 85 and would have created a Medicare bonus on the combined billing ($1.4M), resulting in many thousands of dollars in incentive payments.
There are multiple factors that affect the submission choice; it is truly a case-by-case matter and some creativity is often required to determine the optimal method for any particular practice.
Avoid this top MIPS mistake by taking the time to analyze the situation. Making an informed decision could mean the difference of tens of thousands of dollars for your practice.
Feeling lost? Contact us today! (216) 503-0333.


